Dysphagia. Swallowing difficulty. Esophageal dysphagia. Aspiration risk. Cross section of a human head with Esophagus, Trachea, Nasal cavity, Tongue, Epiglottis, and Food bolus. Healthy and Unhealthy people that have difficulty in swallowing, and the inhalation of fluid while drinking. Medical diagnosis. Detailed vector. Isometric Flat illustration. Schematic diagram
Achalasia is a rare disorder that affects the esophagus, where the muscles of the esophagus do not work properly, and the lower esophageal sphincter (LES) fails to relax, making it difficult for food and liquids to pass into the stomach. This leads to difficulty swallowing, chest pain, and regurgitation of food.
Causes:
The exact cause of achalasia is unknown, but the following factors contribute to its development:
- Nerve Damage: The loss of nerve cells in the esophagus leads to poor muscle function and the inability to relax the LES.
- Autoimmune Response: The body’s immune system may mistakenly attack nerve cells in the esophagus.
- Viral Infections: Some studies suggest that viral infections may contribute to nerve degeneration in the esophagus.
- Genetic Factors: In some cases, there may be a genetic predisposition to developing achalasia.
Risk Factors:
- Age: Achalasia can occur at any age but is most common in people between the ages of 25 and 60.
- Family History: Though rare, a family history of achalasia may increase the risk.
- Autoimmune Disorders: Conditions that affect the immune system can increase the likelihood of developing achalasia.
Symptoms:
- Difficulty Swallowing (Dysphagia): The most common symptom, with a feeling of food getting stuck in the throat or chest.
- Regurgitation of Undigested Food: Food may come back up after eating, especially when lying down.
- Chest Pain: Pain or discomfort in the chest, often confused with heart-related issues.
- Heartburn: A sensation similar to acid reflux.
- Weight Loss: Unintended weight loss due to difficulty eating.
- Coughing or Aspiration: Food or liquids can accidentally enter the lungs, causing coughing or even pneumonia.
- Bloating or Fullness: Feeling bloated or full even after small meals.
Prevention:
There is no definitive way to prevent achalasia, as the causes are largely unknown. However, managing conditions that may contribute to nerve damage (such as autoimmune disorders) and seeking early treatment for swallowing difficulties may help in early diagnosis and management.
Diagnosis:
- Esophageal Manometry: This test measures muscle contractions in the esophagus and assesses the function of the lower esophageal sphincter.
- Barium Swallow X-ray: After swallowing a barium solution, X-rays are taken to observe how liquid moves through the esophagus.
- Endoscopy: A thin, flexible tube with a camera is used to visually inspect the esophagus and rule out other conditions, such as tumors or obstructions.
- Imaging Tests (CT Scans or MRI): These tests may be used to rule out conditions that mimic achalasia, such as cancers or structural abnormalities.
Home Remedies:
- Eat Small, Frequent Meals: Avoid overloading the esophagus by eating smaller portions more frequently.
- Soft and Liquid Diet: Consuming softer foods and liquids can make swallowing easier.
- Drink Water with Meals: Drinking water may help food pass through the esophagus more easily.
- Avoid Spicy and Acidic Foods: These may irritate the esophagus and worsen symptoms.
- Chewing Thoroughly: Chewing food well before swallowing can reduce the risk of food getting stuck.
- Positioning: Stay upright after meals to prevent regurgitation.
Treatment:
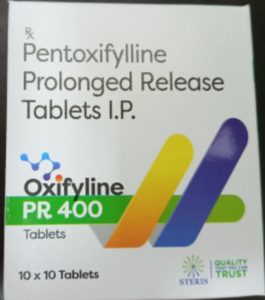
- Medications:
- Nitrates or Calcium Channel Blockers: These medications relax the lower esophageal sphincter, allowing food to pass more easily.
- Pneumatic Dilation: A balloon is inserted and inflated at the lower esophageal sphincter to widen the opening.
- Botox Injections: Botox can be injected into the LES to temporarily relax the muscles and improve swallowing.
- Heller Myotomy: A surgical procedure where the muscles of the LES are cut to allow food to pass into the stomach.
- Peroral Endoscopic Myotomy (POEM): A minimally invasive procedure using an endoscope to cut the LES muscles.
- Esophagectomy: In severe cases, where other treatments fail, part or all of the esophagus may be surgically removed.
Precautions:
- Avoid Large Meals: Eating large meals can increase the pressure in the esophagus and lead to symptoms like regurgitation.
- Stay Upright After Eating: Remain upright for at least 1-2 hours after meals to prevent food from coming back up.
- Avoid Alcohol and Tobacco: Both can worsen the symptoms of achalasia by irritating the esophagus.
- Monitor for Aspiration: Watch for signs of aspiration, such as coughing or choking after eating, which can lead to lung infections.
- Follow Treatment Plans: Adhere to medications or therapies prescribed by your doctor to manage symptoms effectively.
Self-Care:
- Dietary Adjustments: Stick to soft, liquid, or blended foods and avoid dry or tough foods.
- Stay Hydrated: Drinking water throughout meals helps flush food through the esophagus.
- Exercise Moderation: Avoid vigorous physical activity after eating to prevent regurgitation.
- Sleep with Head Elevated: Use a wedge pillow to keep the head elevated during sleep to prevent nighttime regurgitation.
- Regular Monitoring: Regular check-ups with a gastroenterologist to track the progression of symptoms and adjust treatments as needed.
Disclaimer:
Achalasia is a chronic condition that requires medical diagnosis and treatment. While home remedies and self-care strategies can alleviate symptoms, they cannot cure the underlying problem. Consult a healthcare professional for a proper diagnosis and a personalized treatment plan. Attempting to self-diagnose or self-treat can lead to complications like malnutrition or aspiration pneumonia. Always follow your doctor’s advice and seek medical attention if your symptoms worsen or new issues arise.