Doctor with magnifying glass showing model of unhealthy lower rectum on light blue background, closeup. Hemorrhoid problem
Anal fissures are small tears or cracks in the lining of the anus, typically caused by trauma or injury to the anal canal. These fissures can result in pain, discomfort, and bleeding during or after bowel movements. They are common and often heal on their own with proper care.
Causes:
- Constipation: Passing hard or large stools can tear the delicate tissue of the anal canal.
- Diarrhea: Frequent loose stools can cause irritation and lead to fissures.
- Straining During Bowel Movements: Excess pressure on the anal muscles can cause tears.
- Childbirth: Increased pressure during vaginal delivery can lead to fissures.
- Anal Trauma: Injury to the anal region due to foreign objects or anal sex.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease can cause chronic inflammation and fissures.
- Decreased Blood Flow: Reduced blood flow to the anal region, often seen in older adults, can delay healing and increase the risk of fissures.
Risk Factors:
- Chronic Constipation or Diarrhea: Frequent bowel movement issues increase the risk of fissures.
- Childbirth: Women who deliver vaginally are more prone to developing fissures.
- Infants and Young Children: Fissures are common in children, especially those who are constipated.
- Older Adults: Aging reduces blood flow to the anal region, which may slow healing.
- Anal Sex: Can sometimes cause trauma to the anal lining.
- Underlying Conditions: Conditions like Crohn’s disease or HIV increase the risk of fissures.
Symptoms:
- Pain During Bowel Movements: A sharp or burning pain that may last for hours after defecation.
- Bright Red Blood: Blood may appear on toilet paper or in the stool.
- Itching or Irritation: Persistent discomfort or itching around the anus.
- Visible Tear: A small tear or crack may be visible in the skin near the anus.
- Anal Spasms: The muscles around the anus may spasm, causing additional pain.
Prevention:
- Eat a High-Fiber Diet: Foods like fruits, vegetables, and whole grains help keep stools soft and regular.
- Stay Hydrated: Drinking plenty of water prevents hard stools and constipation.
- Avoid Straining: Do not push hard during bowel movements, as it can lead to tears.
- Exercise Regularly: Physical activity promotes good digestion and regular bowel movements.
- Proper Toilet Habits: Respond to the urge to have a bowel movement immediately, and do not delay.
- Good Anal Hygiene: Gently clean the anal area and avoid excessive wiping or harsh soaps.
Diagnosis:
- Physical Examination: A doctor will examine the anal area for visible tears or fissures.
- Anoscopy: A small instrument is used to look inside the anal canal and confirm the presence of a fissure.
- Digital Rectal Exam: A gloved finger may be used to assess for tenderness, but this is often avoided if the pain is severe.
- Additional Tests: In cases of chronic fissures, tests such as colonoscopy may be done to rule out other conditions like inflammatory bowel disease (IBD).
Home Remedies:
- Sitz Baths: Soak in warm water for 10-15 minutes, several times a day, especially after bowel movements, to relax the anal muscles and promote healing.
- Topical Creams: Over-the-counter creams containing hydrocortisone or lidocaine can help relieve pain and inflammation.
- Coconut Oil: Applying coconut oil may soothe the area and promote healing.
- Aloe Vera: Known for its healing properties, aloe vera gel can reduce irritation and promote healing of the fissure.
- High-Fiber Diet: Include fiber-rich foods to soften stools and make bowel movements easier.
- Stool Softeners: Using over-the-counter stool softeners can help prevent straining.
- Hydration: Drink at least 8 glasses of water per day to keep stools soft.
Treatment:
- Dietary Changes: Increase fiber intake to soften stools and avoid straining.
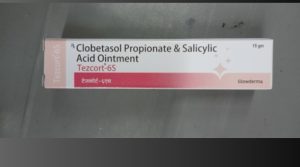
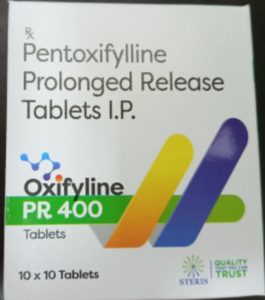
- Topical Medications: Prescription creams such as nitroglycerin ointment or calcium channel blockers help relax the anal sphincter and improve blood flow.
- Botox Injections: Botox may be injected into the anal sphincter to reduce muscle spasms and promote healing.
- Stool Softeners or Laxatives: These help prevent hard stools and reduce the risk of re-tearing the fissure.
- Surgical Options: For chronic or non-healing fissures, a lateral internal sphincterotomy may be recommended, where part of the anal sphincter is cut to reduce pressure and allow the fissure to heal.
Precautions:
- Avoid Straining During Bowel Movements: Use stool softeners if necessary to prevent hard stools.
- Keep the Area Clean: Gently clean the anal area with water and pat dry to avoid irritation.
- Avoid Harsh Wiping: Use soft toilet paper or baby wipes to prevent further trauma to the area.
- Follow Medical Advice: Adhere to prescribed treatments and visit your doctor if symptoms persist or worsen.
Self-Care:
- Sitz Baths: Regularly soak in warm water to relax the muscles and reduce discomfort.
- Maintain a High-Fiber Diet: Include plenty of fruits, vegetables, and whole grains in your diet.
- Stay Hydrated: Drink plenty of fluids to help with digestion and soften stools.
- Avoid Straining: Use laxatives or stool softeners if you experience constipation.
- Use Topical Creams: Apply over-the-counter creams or prescribed ointments to reduce pain and promote healing.
- Avoid Heavy Lifting: Strenuous activities can increase pressure on the anal region.
Disclaimer:
While anal fissures are common and often treatable with home remedies, persistent or severe cases require medical attention. Self-diagnosis and treatment may provide temporary relief, but for long-term or recurring fissures, it’s important to consult a healthcare professional for accurate diagnosis and appropriate treatment. Always follow the guidance of your doctor, especially if your symptoms worsen or do not improve with self-care.