Doctor with magnifying glass showing model of unhealthy lower rectum on light blue background, closeup. Hemorrhoid problem
Anal Fissures
An anal fissure is a small tear or cut in the lining of the anus, typically causing pain and bleeding during or after bowel movements. It can affect people of any age but is particularly common in infants and middle-aged adults.
Causes:
Anal fissures are generally caused by trauma or injury to the anal canal. Common causes include:
- Passing Large or Hard Stools: This is the most frequent cause, often due to constipation.
- Chronic Diarrhea: Repeated loose stools can irritate the anal lining.
- Straining During Bowel Movements: Can cause increased pressure and lead to tearing.
- Childbirth: Straining during labor can cause fissures.
- Anal Intercourse: Can cause trauma to the sensitive lining.
- Inflammatory Bowel Diseases: Conditions like Crohn’s disease increase the risk due to chronic inflammation.
- Tight Anal Sphincter Muscle: In some cases, a tight or overly tense anal sphincter muscle may contribute to fissure formation.
Symptoms:
- Sharp Pain: Pain during or after bowel movements, which can be severe. The pain can last from a few minutes to several hours.
- Bleeding: Bright red blood seen on toilet paper or in the stool.
- Itching or Irritation: The area around the anus may feel itchy or irritated.
- Visible Tear: In some cases, the fissure may be visible as a small cut or tear.
- Spasms: Some people experience muscle spasms in the anal sphincter after a bowel movement.
Diagnosis:
- Physical Examination: A healthcare provider will examine the area around the anus to check for visible tears or cuts.
- Medical History: Discussion of symptoms and any potential triggers like constipation or diarrhea.
- Anoscopy: In some cases, a small scope may be used to inspect the anal canal.
Treatment:
Conservative Treatments:
- Dietary Changes: A high-fiber diet (fruits, vegetables, whole grains) and increased fluid intake can soften stools and reduce straining.
- Stool Softeners: These can make stools easier to pass.
- Sitz Baths: Soaking the anal area in warm water for 10–20 minutes, several times a day, helps relax the muscles and promote healing.
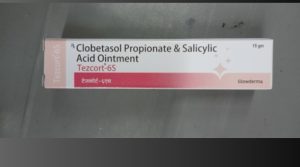
- Topical Medications:
- Numbing Creams (e.g., lidocaine): To reduce pain.
- Nitroglycerin Ointment: Can help relax the sphincter muscle and increase blood flow, promoting healing.
- Calcium Channel Blockers: Creams like diltiazem may also help relax the muscles.
- Steroid Creams: To reduce inflammation and swelling.
Medical Treatments:
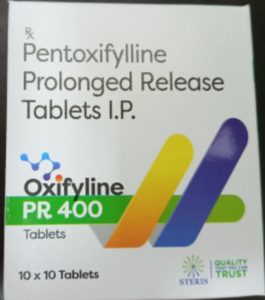
- Botox Injections: Botox can be injected into the sphincter muscle to temporarily paralyze it, reducing spasms and promoting healing.
- Surgical Treatment:
- Lateral Internal Sphincterotomy (LIS): This is a surgical procedure where a small portion of the sphincter muscle is cut to reduce tension, improve blood flow, and allow the fissure to heal. It is usually considered when conservative treatments fail and has a high success rate.
Prevention:
- Prevent Constipation: Regular intake of fiber-rich foods and staying hydrated helps maintain softer stools and reduces the need to strain.
- Gentle Hygiene: Avoid irritating the anal area by using gentle cleaning methods after bowel movements.
- Prompt Treatment: Treating constipation or diarrhea early can prevent the recurrence of fissures.
When to See a Doctor:
- If the pain and bleeding persist despite home treatments.
- If the fissure doesn’t heal within 6–8 weeks (chronic fissure).
- If the fissure recurs frequently or is associated with other symptoms, such as fever, which could indicate an underlying condition like inflammatory bowel disease or infection.
Anal fissures can be very painful, but with proper care and treatment, most fissures heal without the need for surgery.