Selective focus. Patient's hand with an infusion tube. Health care, medicine concept. Copy space composition
Extravasation
What is Extravasation?
Extravasation is the accidental leakage of intravenous (IV) fluids or medications into the surrounding tissue instead of the vein. It usually occurs when the IV catheter punctures or damages the blood vessel, causing the fluid to escape into the nearby tissues. This can cause tissue damage, pain, and other complications, depending on the type of medication that leaks. Extravasation is most concerning when it involves vesicant drugs, which are substances that can cause severe tissue damage.
Types of Extravasation:
- Infiltration: When non-vesicant fluids (those that don’t cause blisters or tissue injury) leak into surrounding tissues, it’s called infiltration. This type usually causes less damage.
- Vesicant Extravasation: Leakage of vesicant drugs, which can cause tissue necrosis (death) and blistering. Common vesicants include chemotherapy drugs, some antibiotics, and calcium chloride.
- Non-Vesicant Extravasation: When non-vesicant medications leak into tissues, it causes mild discomfort or swelling but typically no long-term damage.
Main Causes of Extravasation:
- Poor IV Insertion: Improper placement of the IV catheter can increase the risk of extravasation.
- Fragile Veins: Patients with small or fragile veins, such as the elderly or those with certain medical conditions, are at a higher risk.
- Unsecured IV Catheter: If the IV catheter is not properly secured, it can move, puncturing the vein and causing leakage.
- High-Pressure Infusion: Administering medications under high pressure can damage the blood vessel and lead to extravasation.
- Prolonged Use of the Same IV Site: Repeated or long-term use of the same IV site increases the likelihood of vein damage.
Signs and Symptoms of Extravasation:
- Pain or Burning Sensation: The patient may feel pain, burning, or discomfort at the IV site.
- Swelling: A noticeable swelling around the IV insertion site, which can be due to fluid leakage.
- Redness or Blanching: The skin around the site may become red, or in some cases, it may appear pale or white (blanching).
- Cool Skin: The area may feel cool to the touch due to the presence of IV fluid in the tissue.
- Blisters or Ulcers: In severe cases involving vesicant drugs, blisters or open sores can form.
Risk Factors for Extravasation:
- Age: Older adults, especially those with fragile or thin veins, are at greater risk.
- Multiple IV Attempts: Patients who have had several failed attempts at IV insertion are more likely to experience extravasation.
- Type of Medication: Vesicant drugs, such as certain chemotherapy agents, significantly increase the risk of severe complications if extravasation occurs.
- Prolonged Infusions: Long infusions or repeated infusions at the same site increase the chance of extravasation.
- Peripheral IV Sites: IVs placed in small or fragile veins, especially in the hand or wrist, are more prone to extravasation.
How to Prevent Extravasation:
- Proper IV Placement: Ensure the IV is placed correctly and securely, particularly when administering vesicant drugs.
- Monitor the IV Site: Regularly check the IV site for signs of leakage, such as redness, swelling, or pain.
- Use Central Venous Access: For high-risk drugs, consider using central venous catheters (CVCs) instead of peripheral IVs to reduce the risk of extravasation.
- Educate the Patient: Teach the patient to report any discomfort or unusual sensations at the IV site immediately.
- Use Low Pressure: Administer medications slowly and under low pressure to reduce the likelihood of vein rupture.
How Extravasation is Diagnosed:
- Clinical Examination: Healthcare professionals will assess the IV site for symptoms such as swelling, pain, redness, or coolness.
- Patient Reporting: Patients often report discomfort, burning, or unusual sensations around the IV site, which can help in identifying extravasation early.
- Visual Signs: Visible changes like blisters, skin discoloration, or ulceration may indicate more severe extravasation.
- Ultrasound: In some cases, an ultrasound may be used to confirm the extent of the tissue damage.
Treatment for Extravasation:
- Stop the Infusion Immediately: The first step is to stop the infusion as soon as extravasation is detected.
- Aspiration: Attempt to aspirate as much of the leaked fluid from the site as possible with a syringe.
- Elevation: Elevate the affected limb to reduce swelling and promote fluid drainage.
- Cold or Warm Compresses: Depending on the type of drug extravasated, cold or warm compresses may be applied. Cold is used for vasoconstriction, while warmth can promote absorption of certain medications.
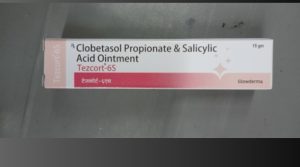
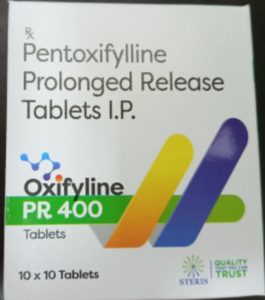
- Antidote Administration: For vesicant drugs, specific antidotes may be injected at the site to neutralize the harmful effects. Examples include hyaluronidase, dimethyl sulfoxide (DMSO), or sodium thiosulfate.
- Surgical Intervention: In severe cases where tissue damage is extensive, surgical debridement or skin grafting may be necessary.
Home Remedies for Extravasation:
- Rest the Affected Area: Keep the area still and elevated to reduce swelling.
- Cool Compresses: Apply cool compresses to the affected area for pain relief and to limit further damage.
- Over-the-Counter Pain Relief: Ibuprofen or acetaminophen can be used to manage discomfort, but always consult a doctor for recommendations.
Ayurvedic Medicine for Extravasation:
While Ayurveda doesn’t directly address extravasation, treatments focused on reducing inflammation and promoting tissue healing can be helpful. Some Ayurvedic approaches include:
- Turmeric: Known for its anti-inflammatory properties, turmeric paste can be applied topically to reduce swelling and pain.
- Aloe Vera: Aloe vera gel has cooling and healing properties, and may be used to soothe the affected area.
- Neem Oil: Neem is known for its antibacterial and anti-inflammatory properties, and can help prevent infection and aid in healing.
- Ashwagandha: Taken orally, ashwagandha can support the immune system and reduce inflammation systemically.
Precautions:
- Monitor IV Sites: Continuously check IV sites for early signs of leakage, especially when administering high-risk medications.
- Use Central Lines: Consider central venous lines for patients receiving vesicant drugs, as they are less prone to extravasation.
- Rotate IV Sites: Regularly change IV sites, especially if there are any signs of irritation or wear at the insertion point.
Self-Care Tips:
- Report Symptoms Early: If you notice any discomfort, swelling, or unusual symptoms around the IV site, report it immediately.
- Elevate the Limb: Keeping the affected limb elevated can help reduce swelling and speed up recovery.
- Stay Hydrated: Keeping well-hydrated can improve circulation and help flush out any fluids that may have leaked into the tissue.
Conclusion:
Extravasation is a potentially serious complication of IV therapy, particularly when vesicant drugs are involved. Early detection and immediate action are crucial in minimizing tissue damage. With proper preventive measures, careful monitoring, and timely intervention, most cases of extravasation can be managed effectively. Healthcare professionals must be vigilant in IV care, while patients should be aware of the signs and symptoms to report promptly.
Disclaimer:
This information is for educational purposes only and should not replace professional medical advice. If you experience any symptoms of extravasation or other complications from IV therapy, seek medical attention immediately.
Additional Tips:
- Use Small Needles: Use the smallest gauge needle possible for vesicant drugs to reduce the risk of damage to the vein.
- Follow Infusion Protocols: Healthcare providers should follow established guidelines for vesicant drug administration to reduce the risk of extravasation.
- Apply Antidote Early: If an antidote is required for the extravasated drug, it should be administered as quickly as possible to minimize tissue damage.