Boy with rosy red cheeks- diathesis or allergy symptoms. Redness and peeling of the skin on the face.
Eczema
What is Eczema?
Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by inflamed, itchy, and red patches of skin. It is most common in infants and children, but it can also occur in adults. Eczema is often associated with other allergic conditions, such as asthma or hay fever. Although the exact cause is unknown, it is thought to be a combination of genetic and environmental factors, leading to an overactive immune response.
Types of Eczema:
- Atopic Dermatitis: The most common form of eczema, often beginning in childhood, it is related to allergies and asthma.
- Contact Dermatitis: Caused by exposure to irritants or allergens like soaps, cosmetics, or plants (e.g., poison ivy).
- Dyshidrotic Eczema: Characterized by small, itchy blisters on the hands and feet.
- Nummular Eczema: Presents as circular, coin-shaped patches of inflamed skin, often triggered by dry skin or allergens.
- Seborrheic Dermatitis: Affects oily areas of the body like the scalp and face, commonly known as dandruff in its milder form.
- Stasis Dermatitis: Typically occurs in the lower legs and is caused by poor circulation.
Main Causes of Eczema:
- Genetics: A family history of eczema, asthma, or other allergic conditions increases the risk.
- Immune System: An overactive immune response to irritants or allergens contributes to inflammation.
- Environmental Triggers: Dry air, extreme temperatures, pollen, dust mites, pet dander, and chemical irritants can trigger flare-ups.
- Skin Barrier Dysfunction: People with eczema tend to have a defective skin barrier, which allows moisture to escape and irritants to enter.
Signs and Symptoms of Eczema:
- Itchy Skin: The most prominent symptom, often worsening at night.
- Red, Inflamed Skin: Affected areas appear red or darker, depending on skin tone.
- Dry, Scaly Patches: The skin becomes dry, cracked, or scaly, especially during flare-ups.
- Oozing or Crusting: In severe cases, the skin may blister and ooze fluid, which can crust over.
- Thickened Skin: Chronic scratching can cause the skin to thicken and become leathery over time.
Risk Factors for Eczema:
- Family History: A genetic predisposition to allergies or asthma increases the likelihood of eczema.
- Allergies: Those with hay fever, asthma, or food allergies are more likely to develop eczema.
- Climate: Cold, dry climates or areas with high pollution can trigger or worsen eczema.
- Stress: Emotional stress can exacerbate eczema symptoms, leading to flare-ups.
- Occupational Exposure: Jobs that involve frequent contact with water, chemicals, or irritants (e.g., healthcare workers, hairdressers) can increase the risk.
How to Prevent Eczema:
- Moisturize Daily: Use fragrance-free creams or ointments to lock in moisture and strengthen the skin’s barrier.
- Avoid Triggers: Identify and avoid common triggers like harsh soaps, allergens, and environmental factors.
- Wear Soft, Breathable Fabrics: Opt for cotton or other soft fabrics that allow the skin to breathe.
- Use Gentle Cleansers: Choose mild, unscented soaps and cleansers to avoid irritating the skin.
- Keep the Skin Hydrated: Drink plenty of water to maintain skin hydration from the inside.
How to Eczema is Diagnosed:
- Physical Examination: A healthcare provider will examine the affected areas and ask about symptoms and possible triggers.
- Medical History: Information about family history of allergies, asthma, or eczema is relevant to diagnosis.
- Patch Testing: If contact dermatitis is suspected, patch testing may be done to identify allergens.
- Skin Biopsy: In rare cases, a small sample of skin may be taken for laboratory analysis to rule out other skin conditions.
Treatment for Eczema:
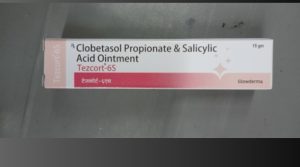
- Topical Corticosteroids: Creams or ointments containing steroids are often prescribed to reduce inflammation and itching.
- Calcineurin Inhibitors: Non-steroidal creams, such as tacrolimus or pimecrolimus, help suppress the immune response and manage symptoms.
- Antihistamines: Oral antihistamines may help reduce itching, especially at night.
- Moisturizers: Emollients are essential to keep the skin hydrated and protect the skin barrier.
- Phototherapy: Light therapy, such as ultraviolet B (UVB) light, can help reduce inflammation in severe cases.
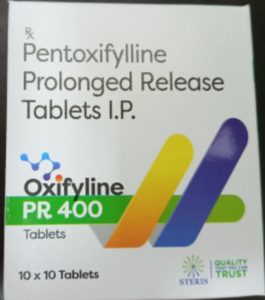
- Systemic Medications: In cases of severe eczema, oral or injectable medications such as biologics (e.g., dupilumab) may be prescribed.
Home Remedies for Eczema:
- Oatmeal Baths: Adding colloidal oatmeal to lukewarm baths can soothe inflamed and itchy skin.
- Coconut Oil: Applying virgin coconut oil may help hydrate the skin and reduce inflammation.
- Aloe Vera: Aloe vera gel can provide a cooling effect and help soothe irritated skin.
- Baking Soda: A baking soda paste applied to the skin can help reduce itching and inflammation.
- Apple Cider Vinegar: Diluted apple cider vinegar can help restore the skin’s pH and reduce irritation.
Ayurvedic Medicine for Eczema:
- Neem (Azadirachta indica): Known for its antibacterial and antifungal properties, neem oil or paste is applied to affected areas to reduce inflammation.
- Turmeric (Curcuma longa): With its anti-inflammatory and antioxidant properties, turmeric can be applied topically or consumed to help manage eczema symptoms.
- Manjistha (Rubia cordifolia): A blood purifier in Ayurveda, it helps clear toxins from the body and improves skin health.
- Aloe Vera (Ghritkumari): Aloe vera is often used in Ayurveda to cool and soothe irritated skin.
- Triphala: Used to detoxify the body and support healthy skin, Triphala may help manage chronic eczema.
Precautions:
- Avoid Hot Showers: Hot water can strip the skin of its natural oils, worsening dryness and irritation.
- Pat Skin Dry: After bathing, gently pat the skin dry instead of rubbing to avoid aggravating the condition.
- Avoid Scratching: Scratching can lead to skin damage and infection. Keep nails trimmed and wear gloves at night if necessary.
- Dress in Layers: Sudden temperature changes can trigger flare-ups, so dress in layers to regulate body heat.
Self-Care Tips:
- Maintain a Skincare Routine: Establish a consistent routine using moisturizers and prescribed treatments to keep symptoms under control.
- Keep a Diary: Track potential triggers, such as foods, environmental factors, or stress, to identify patterns.
- Stay Hydrated: Drink enough water daily to keep your skin hydrated from within.
- Reduce Stress: Practice relaxation techniques, such as yoga, meditation, or breathing exercises, to reduce the impact of stress on your skin.
Conclusion:
Eczema is a chronic condition that can cause discomfort and frustration, but with proper care and treatment, flare-ups can be minimized, and symptoms can be managed. Moisturizing the skin regularly, avoiding triggers, and following prescribed treatments can greatly improve the quality of life for those with eczema. Early intervention and a comprehensive care plan can help prevent complications and manage flare-ups effectively.
Disclaimer:
This information is provided for educational purposes only and should not replace professional medical advice. Always consult a healthcare provider for the diagnosis and treatment of eczema or any other skin condition.
Additional Tips:
- Use a Humidifier: A humidifier can add moisture to the air, preventing dry skin in colder months.
- Patch Test New Products: Before using new skincare products or detergents, test them on a small area of skin to ensure they won’t cause irritation.
- Eat an Anti-Inflammatory Diet: A diet rich in fruits, vegetables, and omega-3 fatty acids may help reduce inflammation and improve skin health.