thermal burn of second degree injury of skin
Cellulitis
What is Cellulitis?
Cellulitis is a common bacterial skin infection that affects the deeper layers of the skin, including the dermis and subcutaneous tissue. It typically occurs when bacteria, most often Streptococcus or Staphylococcus, enter the skin through a cut, scrape, or wound. Cellulitis can cause the skin to become red, swollen, warm, and painful, and it may spread quickly if not treated. While cellulitis can occur anywhere on the body, it is most common on the legs, arms, and face.
Types of Cellulitis:
- Facial Cellulitis: Often affects the skin around the eyes, nose, and cheeks, more commonly seen in children and older adults.
- Periorbital (Preseptal) Cellulitis: A type of facial cellulitis that affects the eyelid and the skin around the eyes, typically due to sinus infections or minor eye injuries.
- Orbital Cellulitis: A more serious infection that spreads deeper into the tissues behind the eyes, requiring immediate medical attention.
- Breast Cellulitis: Can occur following breast surgery or in women with conditions like mastitis.
- Perianal Cellulitis: Affects the skin around the anus, often seen in children, and may be linked to strep infections.
Main Causes of Cellulitis:
- Bacterial Infections: Streptococcus and Staphylococcus bacteria are the most common culprits. In some cases, Methicillin-resistant Staphylococcus aureus (MRSA) can cause more severe cellulitis.
- Cuts and Scrapes: Any break in the skin, such as cuts, scrapes, burns, or surgical wounds, can allow bacteria to enter and cause cellulitis.
- Animal Bites: Bites from animals or humans can introduce bacteria into the skin, leading to cellulitis.
- Skin Conditions: Conditions that cause skin breakdown, such as eczema, athlete’s foot, or ulcers, increase the risk of developing cellulitis.
- Weakened Immune System: People with compromised immune systems, due to conditions like diabetes, HIV, or cancer, are more susceptible to infections like cellulitis.
Signs and Symptoms of Cellulitis:
- Redness and Swelling: The affected area of skin becomes red and swollen.
- Warmth: The skin may feel warm to the touch in the infected area.
- Pain or Tenderness: The affected skin can be painful, particularly when touched.
- Fever: In more severe cases, cellulitis can cause a fever, chills, and fatigue.
- Blisters or Skin Breakdown: Some cases of cellulitis may cause blistering or pus-filled sores.
- Swollen Lymph Nodes: Lymph nodes near the infection site may become swollen as the body tries to fight off the infection.
Risk Factors for Cellulitis:
- Skin Injuries: Any break in the skin increases the risk of bacteria entering and causing infection.
- Chronic Conditions: People with conditions such as diabetes, lymphedema, or poor circulation are at a higher risk of developing cellulitis.
- Weakened Immune System: Immunocompromised individuals, such as those undergoing chemotherapy or taking immunosuppressant drugs, are more prone to infections.
- Obesity: Being overweight can increase the risk of cellulitis, especially in the legs.
- History of Cellulitis: Individuals who have had cellulitis before are more likely to develop it again.
How to Prevent Cellulitis:
- Practice Good Hygiene: Clean any cuts, scrapes, or wounds immediately and cover them with a clean bandage.
- Moisturize: Keeping skin hydrated can prevent cracking, which may allow bacteria to enter.
- Treat Skin Conditions: Properly manage conditions like athlete’s foot or eczema, which can lead to skin breaks and increase infection risk.
- Avoid Walking Barefoot: Particularly in public places, walking barefoot can expose the skin to bacteria.
- Manage Chronic Conditions: If you have diabetes or poor circulation, managing your condition can help lower the risk of cellulitis.
How Cellulitis is Diagnosed:
- Physical Examination: A doctor will assess the affected area for redness, swelling, warmth, and tenderness.
- Medical History: Information about recent injuries, skin conditions, or past infections will be collected.
- Blood Tests: Blood tests may be ordered if the cellulitis is severe or systemic, to check for bacterial infections in the bloodstream.
- Wound Culture: If pus or fluid is present, a sample may be taken to identify the type of bacteria causing the infection.
- Imaging Tests: In some cases, if the infection is deep or in delicate areas like the eyes, imaging tests like an MRI or CT scan may be necessary to assess the extent of the infection.
Treatment for Cellulitis:
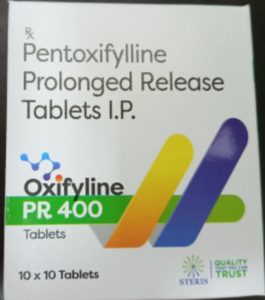
- Antibiotics: Oral antibiotics are usually prescribed to treat the bacterial infection. In more severe cases, intravenous (IV) antibiotics may be necessary.
- Pain Relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can help reduce pain, swelling, and fever.
- Elevate the Affected Area: Elevating the infected limb can help reduce swelling and speed up recovery.
- Hospitalization: In severe cases, especially with systemic symptoms or if the infection spreads rapidly, hospitalization may be necessary for IV antibiotics and close monitoring.
Home Remedies for Cellulitis:
- Warm Compresses: Applying a warm, damp cloth to the infected area may help reduce discomfort and improve circulation.
- Rest and Elevation: Resting and elevating the affected area can reduce swelling and help the body fight the infection.
- Hydration: Drink plenty of water to stay hydrated and support the immune system’s response to the infection.
Ayurvedic Medicine for Cellulitis:
- Turmeric (Curcuma longa): Known for its powerful anti-inflammatory and antibacterial properties, turmeric can be applied topically in a paste or taken internally to help fight infection.
- Neem (Azadirachta indica): Neem leaves or oil can be used to help heal the skin and reduce bacterial infection.
- Manjistha (Rubia cordifolia): Traditionally used to cleanse the blood, manjistha may help in reducing inflammation and fighting infections.
- Triphala: A mixture of three fruits, Triphala is often used in Ayurveda to detoxify the body and support the immune system, helping to fight infections.
Precautions:
- Avoid Scratching or Irritating the Skin: This can worsen the infection or spread it to other parts of the body.
- Complete Antibiotic Course: If prescribed antibiotics, it’s essential to finish the full course, even if the symptoms improve before the medication is finished.
- Seek Immediate Medical Attention for Worsening Symptoms: If the infection spreads, causes fever, or doesn’t improve with treatment, seek immediate medical care.
Self-Care Tips:
- Keep Wounds Clean: Proper wound care is essential to prevent infection from spreading or worsening.
- Wear Loose Clothing: Tight clothing can irritate the infected skin, so opt for loose, breathable fabrics.
- Monitor for Spread: Keep an eye on the infected area to ensure it’s not spreading. Draw a line around the affected area to help track its size.
Conclusion:
Cellulitis is a potentially serious bacterial skin infection that requires prompt medical treatment. While it can be treated effectively with antibiotics, ignoring symptoms or delaying treatment can lead to complications. Preventive measures, such as proper wound care and managing underlying conditions like diabetes, are key to avoiding cellulitis.
Disclaimer:
This information is provided for educational purposes only and is not intended to replace professional medical advice. Always consult a healthcare provider for proper diagnosis and treatment of cellulitis or any other medical condition.
Additional Tips:
- Foot Care: People with diabetes should pay extra attention to foot care, as poor circulation and nerve damage can increase the risk of cellulitis.
- Immediate Care for Bites: Clean animal or insect bites immediately and monitor for signs of infection.
- Strengthen Immune Health: A balanced diet and regular exercise can help support your immune system and reduce the risk of infections like cellulitis.