Young girl with Atopic dermatitis,type of eczema,is an inflammatory, chronically relapsing, non-contagious and pruritic skin disease. It has been given names like "prurigo Besnier," "neurodermitis," "endogenous eczema," "flexural eczema," "infantile eczema," and "prurigo diathsique.
Atopic Dermatitis
What is Atopic Dermatitis?
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. It is part of the “atopic triad,” often associated with asthma and allergic rhinitis (hay fever). Atopic dermatitis tends to flare up periodically and can affect both children and adults.
Types of Atopic Dermatitis:
- Infantile Atopic Dermatitis: Appears in babies, typically affecting the face, scalp, and outer limbs.
- Childhood Atopic Dermatitis: Common in children, affecting the folds of elbows, knees, wrists, and ankles.
- Adult Atopic Dermatitis: In adults, eczema usually affects areas like the hands, neck, and face.
- Nummular Eczema: Circular, coin-shaped patches of eczema.
- Dyshidrotic Eczema: A form affecting the hands and feet, causing small blisters and intense itching.
Main Causes of Atopic Dermatitis:
- Genetic Factors: Family history of eczema, asthma, or allergies increases the risk.
- Immune System Dysfunction: An overactive immune response can lead to inflammation and skin irritation.
- Environmental Triggers: Exposure to allergens (dust, pet dander, pollen), harsh soaps, or extreme weather conditions can trigger flare-ups.
- Skin Barrier Dysfunction: People with atopic dermatitis have a weakened skin barrier, causing moisture loss and allowing irritants to penetrate the skin.
- Stress: Emotional stress may exacerbate symptoms.
Signs and Symptoms of Atopic Dermatitis:
- Dry, Itchy Skin: Intense itching, often worsening at night, is a hallmark symptom.
- Red, Inflamed Patches: Red, swollen skin, sometimes accompanied by small bumps or blisters.
- Thickened or Scaly Skin: Chronic eczema may lead to thick, leathery patches known as lichenification.
- Crusting and Oozing: In severe cases, the skin may ooze and crust over from scratching.
- Skin Infections: Repeated scratching can cause open sores, increasing the risk of bacterial infections.
Risk Factors for Atopic Dermatitis:
- Family History: Having close relatives with eczema, asthma, or hay fever increases the risk.
- Living in Urban Areas or Cold Climates: These environments tend to have more allergens and irritants.
- Asthma and Allergies: Individuals with a history of other allergic conditions are at higher risk.
- Early Childhood: Atopic dermatitis is more common in infants and young children.
How to Prevent Atopic Dermatitis:
- Moisturize Regularly: Keep the skin hydrated with emollients to maintain the skin barrier.
- Avoid Triggers: Identify and avoid known allergens, irritants, and triggers such as harsh soaps or detergents.
- Wear Soft Fabrics: Choose clothing made from breathable, natural fibers like cotton to reduce irritation.
- Stay Cool: Keep the skin cool and avoid excessive sweating, as heat and sweat can worsen symptoms.
- Manage Stress: Stress can trigger flare-ups, so practicing relaxation techniques like meditation can help.
How Atopic Dermatitis is Diagnosed:
- Medical History: A thorough history of symptoms, family history of eczema or allergies, and triggers is taken.
- Physical Examination: The doctor will examine the appearance, distribution, and severity of the skin lesions.
- Allergy Testing: In some cases, patch testing or blood tests may be done to identify allergens.
- Skin Biopsy: Rarely, a skin biopsy may be performed to rule out other skin conditions.
Treatment for Atopic Dermatitis:
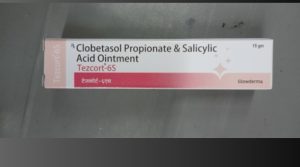
- Topical Steroids: Creams or ointments containing corticosteroids are commonly prescribed to reduce inflammation and itching.
- Topical Calcineurin Inhibitors: Non-steroidal creams like tacrolimus and pimecrolimus help reduce inflammation and are used for sensitive areas.
- Antihistamines: Oral antihistamines can help reduce itching, especially at night.
- Moisturizers: Thick emollients are crucial for keeping the skin hydrated and preventing flare-ups.
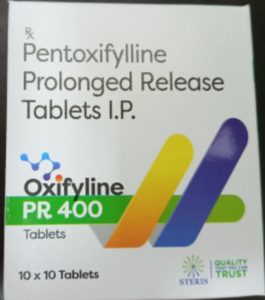
- Immunosuppressive Drugs: For severe cases, medications like cyclosporine or methotrexate may be used to suppress the immune system.
- Light Therapy (Phototherapy): Ultraviolet (UV) light treatment may help reduce inflammation in some patients.
Home Remedies for Atopic Dermatitis:
- Oatmeal Baths: Adding colloidal oatmeal to bathwater can soothe itchy, irritated skin.
- Coconut Oil: Has moisturizing and antimicrobial properties that can help protect the skin.
- Aloe Vera: Its anti-inflammatory properties can soothe irritated skin and promote healing.
- Apple Cider Vinegar: Diluted apple cider vinegar may help restore the skin’s natural acidity and prevent infections.
- Honey: Known for its antibacterial properties, applying honey may help in healing open sores.
Ayurvedic Medicine for Atopic Dermatitis:
- Neem (Azadirachta indica): Known for its anti-inflammatory and antimicrobial properties, neem paste or oil can be applied topically.
- Kumari (Aloe Vera): Aloe vera can soothe the skin and reduce inflammation.
- Turmeric (Curcuma longa): Has anti-inflammatory and antioxidant properties and can be applied as a paste or taken internally.
- Manjistha (Rubia cordifolia): Often used in Ayurveda for skin conditions, manjistha may help purify the blood and reduce eczema symptoms.
- Ashwagandha: Helps reduce stress and anxiety, which can trigger eczema flare-ups.
Precautions:
- Avoid scratching, as it can worsen the condition and lead to infections.
- Use mild, unscented soaps and laundry detergents to avoid irritation.
- Keep fingernails short to minimize damage from scratching.
- Be cautious with over-the-counter creams, especially those containing strong chemicals or fragrances.
Self-Care Tips:
- Use Lukewarm Water: Bathe or shower in lukewarm water, as hot water can dry out the skin and worsen symptoms.
- Pat Skin Dry: After bathing, gently pat the skin dry with a towel and apply moisturizer while the skin is still damp.
- Dress in Layers: Avoid overheating by wearing breathable layers and staying in cool environments.
- Keep Humidity in Check: Use a humidifier to add moisture to the air during dry, cold seasons.
Conclusion:
Atopic dermatitis is a chronic but manageable skin condition that requires a combination of medical treatment, lifestyle adjustments, and proper skincare. Identifying triggers and maintaining skin hydration are key to reducing flare-ups and improving quality of life.
Disclaimer:
The information provided is for educational purposes only and should not replace professional medical advice. Always consult a healthcare provider for proper diagnosis and treatment of atopic dermatitis or any other medical condition.
Additional Tips:
- Consider patch testing to identify allergens that may be triggering flare-ups.
- For infants, avoid potential irritants like wool clothing or harsh soaps.
- Keep skin-care products simple—use products labeled for sensitive skin and avoid those with added fragrances or dyes.