Woman feel pain in stomach concept vector illustration. Stomach acid and digestive system problem.
Acidity (also known as acid reflux or heartburn) occurs when excess gastric acid flows back into the esophagus, causing a burning sensation in the chest or throat. It is a common condition that can range from mild discomfort to severe pain.
Causes:
- Excessive Production of Stomach Acid: Can be triggered by certain foods and drinks like spicy food, fatty meals, alcohol, and caffeine.
- Irregular Eating Habits: Skipping meals or eating large meals can cause acid buildup.
- Obesity: Increases pressure on the stomach, leading to acid reflux.
- Pregnancy: Hormonal changes and pressure on the stomach can lead to acid reflux.
- Smoking: Reduces the function of the lower esophageal sphincter (LES).
- Hiatal Hernia: A condition where the upper part of the stomach pushes into the chest, weakening the LES.
- Medications: Certain medications like NSAIDs, aspirin, and some muscle relaxants can irritate the stomach lining.
Risk Factors:
- Diet: High-fat foods, spicy foods, and beverages like coffee and alcohol.
- Lifestyle: Smoking, lack of exercise, and stress.
- Medical conditions: Hiatal hernia, obesity, or pregnancy.
- Medications: Certain painkillers, antihistamines, and sedatives.
Symptoms:
- Burning sensation in the chest (heartburn).
- Sour taste in the mouth or regurgitation of food.
- Difficulty swallowing.
- Nausea and bloating.
- Hoarseness or a sore throat.
- Dry cough, especially at night.
- Bad breath.
Prevention:
- Healthy Eating: Avoid triggers such as spicy, fried, or acidic foods.
- Smaller Meals: Eat smaller, more frequent meals to prevent overproduction of acid.
- Avoid Lying Down After Eating: Stay upright for at least 2-3 hours after eating.
- Elevate the Head While Sleeping: Raising the head of your bed can prevent acid from moving up the esophagus.
- Weight Management: Maintaining a healthy weight can reduce pressure on the stomach.
- Quit Smoking: Improves the function of the LES.
- Limit Alcohol and Caffeine: Both can increase acid production.
Diagnosis:
- Physical Examination: The doctor may ask about symptoms and medical history.
- Endoscopy: A procedure to examine the esophagus for signs of damage or inflammation.
- pH Monitoring: Measures the amount of acid reflux over 24 hours.
- Esophageal Manometry: Measures the muscle contractions in the esophagus.
Treatment:
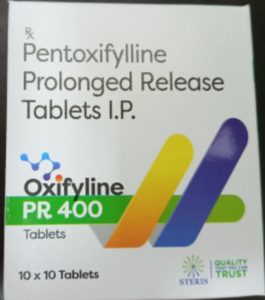
- Antacids: Over-the-counter medications that neutralize stomach acid (e.g., Tums, Rolaids).
- H2 Blockers: Reduce acid production (e.g., ranitidine, famotidine).
- Proton Pump Inhibitors (PPIs): More potent acid reducers (e.g., omeprazole, esomeprazole).
- Lifestyle Changes: Diet modifications, weight loss, and smoking cessation.
- Surgery: In severe cases, surgery like fundoplication may be necessary to strengthen the LES.
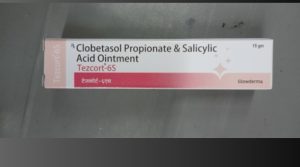
Precautions:
- Avoid Triggers: Identify and avoid foods or habits that worsen acidity.
- Regular Meals: Eat at regular intervals and avoid skipping meals.
- Stress Management: Practice relaxation techniques like yoga or meditation.
- Follow Prescribed Treatment: Ensure adherence to medication schedules if prescribed by a doctor.
Self-Care:
- Home Remedies: Ginger, chamomile tea, and baking soda mixed with water may provide temporary relief.
- Stay Hydrated: Drinking enough water can help neutralize stomach acid.
- Chew Gum: Stimulates saliva production, which can neutralize acid.
- Avoid Tight Clothing: Pressure on the abdomen can worsen reflux.
Disclaimer:
Self-diagnosis and treatment of acidity should be avoided. While home remedies and over-the-counter medications can provide temporary relief, persistent or severe acidity may indicate an underlying condition that requires medical evaluation. Always consult a healthcare professional before starting any treatment plan, especially if symptoms worsen or do not improve with self-care.