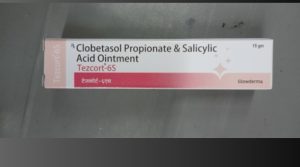
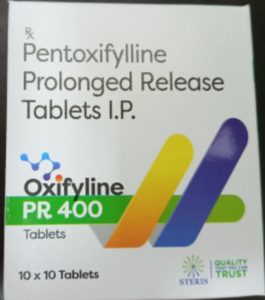
Close-up of medicines in blister packs
Sulfadiazine Overview
Sulfadiazine is a sulfonamide antibiotic primarily used to treat bacterial infections, particularly those caused by susceptible organisms. It acts by inhibiting bacterial folic acid synthesis, essential for DNA replication and cell division. Sulfadiazine is often used in combination with other antibiotics to enhance efficacy and reduce resistance.
Uses/Indications
Sulfadiazine is commonly used for:
- Toxoplasmosis: In combination with pyrimethamine, it’s the drug of choice for treating toxoplasmosis, especially in immunocompromised patients such as those with HIV/AIDS.
- Urinary Tract Infections (UTIs): Effective against susceptible strains of Escherichia coli and Proteus species.
- Meningitis: Used in combination with other antibiotics to treat bacterial meningitis caused by Haemophilus influenzae or Neisseria meningitidis.
- Burn-related Infections: Silver sulfadiazine (a topical form) is used for the prevention and treatment of burn wound infections.
- Rheumatic Fever: Used as long-term prophylaxis to prevent recurrence of rheumatic fever.
Dosage
The dosage of Sulfadiazine varies depending on the indication, age, and weight of the patient:
- For Toxoplasmosis (Adults): Typically, 1 to 1.5 grams of sulfadiazine every 6 hours in combination with pyrimethamine. Pyrimethamine dose is adjusted based on the severity of the infection.
- For UTIs: Initial dose is often 2-4 grams, followed by 1-2 grams every 6 hours for 7-10 days.
- For Meningitis: 75-100 mg/kg/day, divided into 4 doses, with close monitoring.
- Prophylaxis in Rheumatic Fever: 1 gram once a day.
- Topical (Silver Sulfadiazine): Applied once or twice daily to burn wounds.
Pharmacokinetics:
- Absorption: Well absorbed orally.
- Distribution: Widely distributed throughout the body, including cerebrospinal fluid (CSF), pleural fluid, and synovial fluid.
- Metabolism: Partially metabolized in the liver.
- Excretion: Primarily eliminated via the kidneys.
Side Effects
Sulfadiazine can cause various side effects, which may range from mild to severe:
- Hypersensitivity Reactions: Including rash, fever, and urticaria. Severe cases can result in Stevens-Johnson syndrome or toxic epidermal necrolysis (TEN).
- Gastrointestinal Effects: Nausea, vomiting, diarrhea, and abdominal pain.
- Hematologic Effects: Leukopenia, agranulocytosis, thrombocytopenia, and aplastic anemia. It may cause hemolysis in patients with G6PD deficiency.
- Renal Effects: Crystalluria, interstitial nephritis, and kidney stones (particularly with inadequate hydration).
- Hepatotoxicity: Rare cases of liver toxicity may occur.
- Photosensitivity: Increased sensitivity to sunlight, leading to sunburns or skin rashes.
- Kernicterus: In neonates, sulfadiazine can cause kernicterus due to displacement of bilirubin from albumin, leading to neurotoxicity.
Contraindications
Sulfadiazine is contraindicated in:
- Hypersensitivity to sulfonamides.
- Pregnancy and Neonates: Especially in the third trimester, as it increases the risk of kernicterus in the newborn.
- Severe liver or renal impairment: Without appropriate dose adjustment.
- G6PD Deficiency: Risk of hemolytic anemia.
- Porphyria: Can precipitate an acute attack.
Drug Interactions
Sulfadiazine can interact with various drugs:
- Warfarin: Increases the anticoagulant effect, raising the risk of bleeding.
- Methotrexate: Competes for protein binding, potentially increasing methotrexate toxicity.
- Phenytoin: Inhibits the metabolism of phenytoin, leading to increased toxicity.
- Oral Hypoglycemics: May enhance the hypoglycemic effect of sulfonylureas.
- Ciclosporin: Can decrease the effectiveness of ciclosporin in transplant patients, increasing the risk of organ rejection.
- Pyrimethamine: When used together (e.g., in toxoplasmosis treatment), folic acid supplementation may be required due to the risk of bone marrow suppression.
Resistance
Resistance to sulfonamides, including sulfadiazine, has increased over time due to widespread use. Bacterial resistance mechanisms include:
- Increased production of PABA, overcoming the inhibitory effect of sulfonamides.
- Mutations in dihydropteroate synthase, reducing drug binding.
Sulfadiazine is generally less effective against certain bacteria, particularly those that have developed resistance, such as certain strains of Escherichia coli and Staphylococcus aureus.
Special Considerations
- Hydration: To prevent crystalluria and kidney stone formation, patients should maintain adequate hydration during therapy.
- Folic Acid Supplementation: When combined with pyrimethamine (for toxoplasmosis), folic acid supplementation is often required to reduce the risk of bone marrow suppression.
- Monitor Renal and Liver Function: Especially in patients with pre-existing conditions.
- G6PD Deficiency: Screen for G6PD deficiency in patients from regions where it is prevalent before initiating therapy.
- Pediatric Use: Should be avoided in neonates due to the risk of kernicterus.
Conclusion
Sulfadiazine is an effective antibiotic, particularly when used in combination with pyrimethamine for the treatment of toxoplasmosis or other parasitic and bacterial infections. However, its use is limited by the potential for severe side effects, including hypersensitivity reactions and hematologic toxicity, as well as increasing bacterial resistance. Careful monitoring of renal function, blood counts, and drug interactions is essential during treatment. Its use should be avoided in neonates, pregnant women, and individuals with G6PD deficiency.