Horribly dry and infected man's foot.
Athlete’s Foot Overview
Athlete’s foot, also known as tinea pedis, is a common fungal infection that affects the skin on the feet. It typically occurs in warm, moist environments, such as locker rooms, public showers, and swimming pools. The fungus thrives in these areas and can cause a scaly, itchy rash that can spread to other parts of the body if untreated.
Causes
Athlete’s foot is caused by dermatophytes, a group of fungi that live on dead tissue of the skin, hair, and nails. The infection spreads through direct contact with contaminated surfaces or by sharing towels, shoes, or socks with an infected person.
Risk Factors
- Exposure to damp environments: Locker rooms, public showers, and swimming pools are common breeding grounds for the fungus.
- Wearing tight or closed shoes: Shoes that trap moisture and warmth, such as sneakers, increase the risk.
- Sweaty feet: Excessive sweating can create an ideal environment for the fungus to grow.
- Sharing personal items: Using someone else’s towels, shoes, or socks can spread the infection.
- Compromised immune system: People with weakened immune systems (e.g., diabetes, HIV) are more susceptible.
Symptoms
Athlete’s foot can present in different ways, but common symptoms include:
- Itching: Often between the toes.
- Redness and scaling: The skin may become red, flaky, or scaly, especially in the spaces between the toes or on the soles of the feet.
- Cracked skin: Cracks or fissures may develop, leading to pain and discomfort.
- Blisters: In some cases, blisters may form, which can lead to open sores if they burst.
- Thickened or discolored nails: The fungus can also affect the toenails, making them thick, crumbly, or discolored.
Diagnosis
- Visual inspection: A healthcare provider can often diagnose athlete’s foot by examining the affected area.
- Skin scrapings: A small sample of the affected skin may be taken and examined under a microscope to confirm the presence of the fungus.
- Culture test: In some cases, a fungal culture may be done to identify the specific type of fungus.
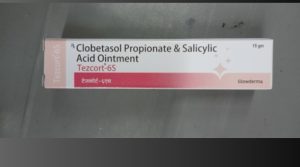
Treatment
- Topical antifungal medications: Athlete’s foot is typically treated with over-the-counter antifungal creams, sprays, or powders, such as:
- Clotrimazole
- Miconazole
- Terbinafine
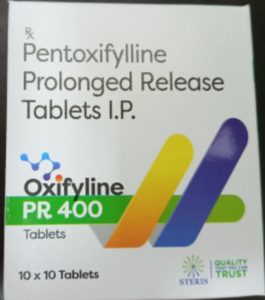
- Oral antifungal medications: In severe cases or when topical treatments fail, oral antifungal drugs like terbinafine or itraconazole may be prescribed.
- Keeping feet dry: Drying the feet thoroughly after washing is essential, especially between the toes.
- Foot powders: Using antifungal or drying powders can help prevent moisture buildup and recurrence.
Complications
If left untreated, athlete’s foot can lead to:
- Spread of infection: The fungus can spread to the toenails (onychomycosis) or other areas of the body, such as the groin (jock itch) or hands.
- Bacterial infections: Cracked skin can become infected with bacteria, leading to more serious conditions like cellulitis.
- Chronic recurrence: Athlete’s foot can become a persistent problem if not properly treated or if the environment that caused it is not addressed.
Precautions and Prevention
- Keep feet clean and dry: Wash your feet daily with soap and water, and dry them thoroughly, especially between the toes.
- Wear breathable shoes: Choose shoes made of materials like leather or canvas, which allow air circulation and reduce moisture buildup.
- Change socks regularly: Wear clean, dry socks, and change them if they become sweaty during the day.
- Use antifungal powders: Applying antifungal powder or spray to your feet and shoes can help prevent infection.
- Wear flip-flops in public places: Avoid going barefoot in locker rooms, public showers, and around pools.
- Don’t share personal items: Avoid sharing towels, shoes, or socks with others.
Self-Care and Management
- Apply antifungal creams: Follow the directions on over-the-counter antifungal products, applying them to the affected areas for the recommended duration, even after symptoms disappear, to prevent recurrence.
- Keep feet dry: Air your feet out when possible, and avoid wearing the same pair of shoes every day. Rotate between pairs to allow them to dry out.
- Practice good foot hygiene: Wash your feet daily, and keep nails trimmed to reduce the risk of fungal growth under the nails.
Athlete’s foot is easily treated and prevented with proper hygiene and prompt use of antifungal products. If symptoms persist or worsen, medical attention may be needed to avoid complications.