asian women suffer from constipation hold and squeezing toilet paper roll sitting in bathroom
Blood in Stool
The presence of blood in the stool can be a concerning symptom and may indicate various underlying conditions. Here’s a detailed overview:
Causes
- Hemorrhoids: Swollen veins in the rectum or anus that can cause bright red blood.
- Anal Fissures: Small tears in the lining of the anus that can lead to bleeding.
- Gastrointestinal Bleeding: Internal bleeding in the stomach, small intestine, or colon.
- Diverticulosis: Pouches in the colon that can bleed.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease or ulcerative colitis that cause inflammation in the digestive tract.
- Peptic Ulcers: Sores in the lining of the stomach or small intestine.
- Colorectal Cancer: Tumors in the colon or rectum can cause bleeding.
- Gastrointestinal Infections: Infections causing inflammation and bleeding.
- Polyps: Non-cancerous growths in the colon or rectum that can bleed.
Risk Factors
- Age: Risk increases with age, especially for conditions like colorectal cancer.
- Family History: A family history of gastrointestinal diseases or cancer.
- Diet: Low-fiber diets and high consumption of red or processed meats.
- Chronic Conditions: Such as IBD or peptic ulcers.
- Lifestyle Factors: Smoking, excessive alcohol consumption, or heavy lifting.
Symptoms
- Bright Red Blood: Often on the surface of stool or on toilet paper, indicating bleeding from the rectum or anus.
- Dark or Black Stool: Indicates bleeding from higher in the digestive tract, such as the stomach.
- Abdominal Pain: Cramping or discomfort in the abdominal area.
- Changes in Stool: Including consistency, color, or frequency.
- Other Symptoms: Weakness, dizziness, or unintentional weight loss.
Diagnosis
- Physical Examination: Including a digital rectal exam to check for external hemorrhoids or fissures.
- Blood Tests: To check for anemia or signs of infection.
- Stool Tests: To identify the presence of blood or pathogens.
- Endoscopy: Such as a colonoscopy or upper endoscopy to visualize and assess the gastrointestinal tract.
- Imaging Studies: CT scans or MRI to evaluate internal structures.
Treatment
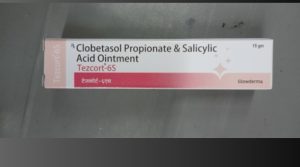
- Hemorrhoids and Anal Fissures: Over-the-counter creams, sitz baths, and dietary changes.
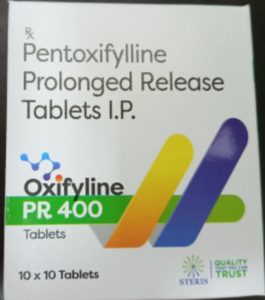
- Inflammatory Bowel Disease: Medication to reduce inflammation and manage symptoms.
- Peptic Ulcers: Acid-reducing medications and antibiotics if an infection is present.
- Diverticulosis: Dietary changes and, if necessary, surgery.
- Colorectal Cancer: Surgery, chemotherapy, or radiation depending on the stage.
- Infections: Antibiotics or antiviral medications as needed.
Complications
- Anemia: Chronic bleeding can lead to anemia due to loss of red blood cells.
- Worsening of Underlying Conditions: Such as progression of cancer or severe inflammation.
- Infections: Complications from untreated infections or inflammatory diseases.
Precautions
- Early Medical Attention: Seek prompt evaluation if blood in stool is observed.
- Regular Screening: Especially if at risk for colorectal cancer or other gastrointestinal issues.
- Dietary Changes: Increase fiber intake and avoid known irritants.
- Avoid Smoking and Excessive Alcohol: Both can exacerbate gastrointestinal problems.
Self-Care
- Maintain a Healthy Diet: High in fiber and low in irritants.
- Stay Hydrated: Drink plenty of fluids.
- Monitor Symptoms: Track any changes in stool, pain, or other symptoms.
- Follow Medical Advice: Adhere to treatment plans and regular check-ups.
Blood in the stool can be a sign of various health issues, some of which may be serious. It is important to seek medical evaluation to determine the cause and receive appropriate treatment.